Diagnostic Workup Guide
We recognize that those experiencing vaccine adverse effects are struggling to get proper diagnosis and care. To date we have not identified one lab result that is applicable to all. Much of what we have seen so far is a diagnosis by exclusion approach, running many labs to see what may turn up positive. Over time, by sharing our results we hope to narrow the scope of testing. We have found the results of standard blood work and imaging are usually unremarkable. The tests mentioned in this document often show positive results amongst our community. We are sharing what we’ve learned in the hopes of expediting the road toward treatment and to rule out/identify any underlying conditions or other diseases that may have re-emerged. This document should be used for reference to guide a diagnostic workup based on individual symptomatology and discussion with specialists. With your medical team, you can determine which tests are the best options based on symptoms. Patients DO NOT need to be tested for every test on this list. This is not a prescriptive list with the indication that all tests should be undertaken. That said, we recognize that many test results are normal and pressing for further investigation is often warranted. Please use this Printable Version for a more in depth review with your medical teams
** This list was not written by a medical institution or doctor. This list is not intended to diagnose, treat, cure or prevent any disease. The considerations offered in this guide do not replace the medical interventions prescribed by the user’s care team and should be evaluated prior to implementation.
In many cases where we encounter a myriad of symptoms such as polyneuropathy, visual disturbances, heart rate variability, digestion issues, dizziness, muscle fasciculations (twitching), etc. we have noted positive testing results suggestive of dysautonomia and sudomotor/small fiber neuropathy. This testing has led to therapeutic treatments for this specific cluster of symptoms. For further information please go to www.react19.org.
Action Plan
HOW TO APPROACH YOUR DOCTOR: Your relationship with your doctor is unique. Consider a new relationship vs an existing/trusted relationship. If you have a good existing relationship with your doctor, your approach will be much more direct and you may consider discussing this guide with them. If it is a new doctor or a doctor you do not have a trusting relationship with, we do not recommend handing them this guide.
1. When discussing with your doctor avoid "self-diagnosing" / insisting that your issues are from the vaccine. Let the timeline and symptoms speak for themselves.
2.Present your symptoms in a clear and concise manner with an an approximate timeline. Explain your level of function before the illness began, then explain illness that ensued / timeline of symptoms. (For example: "I was working out, healthy, then on [x-date] I received my 2nd dose of vaccine, then [x-days] later I woke up with twitching and nausea and tinnitus." )
2a. Document your symptoms in a list with video and photos if possible.
3. Explain to your doctor that you are in contact with a scientific community that is investigating these reactions and we are finding positive tests that have provided a pathway for potential answers and treatments.
3a. Ask your doctor if they would be open to run some of these tests. (For Example: if you are suffering neuropathy, you can say something like: "Some who have neuropathy like me, have a positive skin biopsy test. If you are unable to do this test, would you be able to refer me to a specialist who can run this test?")
FINDING A DOCTOR: Each Doctor is unique and their willingness to help will vary. If you find a doctor unwilling to help you, go for a different doctor. Don't give up, continue to search for a doctor until you find the right fit for you. It is not uncommon for us to cycle through dozens of doctors until you find the right fit for you. Find a doctor HERE Can't find what you're looking for? Contact Us to connect with the advocacy team for more options.
Make appointments with the following doctors:
- PCP (Primary Care Physician) - Neuromuscular Neurologist (confirm they do SFN biopsy, and better if they have a dysautonomia sub-specialty) - Cardiologist - Allergist-Immunologist - Rheumatologist - Hematologist - Infectious Disease - Integrative Medicine
Rule out pre-existing or new conditions:
It’s important to investigate exacerbations of any possible pre-existing medical conditions and the development of any new conditions that are commonly found in post vaccine adverse reactions. -Small fiber neuropathy -Dysautonomia -POTS (Postural orthostatic tachycardia syndrome) -Autoimmune conditions -Gastrointestinal disorders -Post-viral syndromes/latent virus/reactivation -Allergies -Hypermobile EDS -MCAS (Mast cell activation syndrome) -ME/CFS (Myalgic encephalomyelitis / chronic fatigue syndrome)
*Not including more specific blood work for neurology, auto-immunity and cardiovascular. See those in sections 2-4. **Attempt to have PCP order labs in this section during your first visit:
- ANA
- Negative result does NOT rule out auto-immunity
- BNP (Brain natriuretic peptide)
- Heart inflammation - myocarditis
- Complement 3, Complement 4 (C3, C4)
- A non-specific autoimmune marker initially often tested before more advanced testing.
- Complement Total 50 (CH50)
-
Measures the amount and activity of all the major complement proteins often used to diagnose conditions such as lupus and/or rheumatoid arthritis.
- Complete Blood Count (CBC w/ Diff)
- A measure of the number of red blood cells, white blood cells, and platelets in the blood, including the different types of white blood cells (neutrophils, lymphocytes, monocytes, basophils, and eosinophils). Low may be due to acute viral, lowered immune and cortisol.
- Comprehensive Metabolic Panel (CMP)
- Albumin, ALP, ALT, AST, bilirubin, BUN, calcium, carbon dioxide (electrolyte), chloride (electrolyte), creatinine, glucose, potassium (an electrolyte), sodium (an electrolyte), total protein.
- Copper
- Copper HIGH- tied to low zinc. Copper LOW- peripheral neuropathy
- C-Reactive Protein (CRP)
- CRP is produced by the liver. Levels rise when there is inflammation in the body.
- Erythrocyte Sedimentation Rate (Sed Rate -ESR)
- Inflammatory marker
- D-Dimer
- Run D-dimer especially if there are signs or symptoms of blood clotting. Note that D-dimer tests can fluctuate and in the absence of symptoms may have no clinical significance. There are other tests you can run if there is clinical suspicion of clotting disorder: PT/INR, fibrinogen activity, antithrombin antibody. If D-dimer is high, your doctor may also run CH50.
- Ferritin
- LOW dangerous, *We have seen anemia after vaccination. HIGH iron and ferritin are seen in COVID illness. High ferritin was related to COVID severity..
- Clotting Tests Antithrombin antibody, PTT/INR, fibrinogen activity, fibrinogen, plasminogen activator inhibitor-1, TAT complex, plasmin-α2-PI complex, factor V assay, platelet dense granule deficiency, platelet aggregation test.
- These may be considered in cases of clotting symptoms or risks. Aside from PTT/INR and fibrinogen, others are considered in severe cases and/or in the realm of research and may only be considered by a hematologist. Aside from special microscopy, there is no current test widely used for diagnosing microclots.
- Immunoglobulins A, G, M ( IgA, IgG, IgM)
-
If your levels of IgG, IgM, or IgA are too low or too high, your doctor should do follow up testing to determine the cause.
- Homocysteine
-
This test is marker to measure cardiac risk factors. Homocysteine is also used to identify folate, Vitamin B12 deficiency. People with positive MTHFR may be at increased risk of elevated Homocysteine. This test can help identify if you have MTHFR.
- IgE (Immunoglobulin Type E 3)
- HIGH - allergic response
- IgG 1, 2, 3, 4 (Subclasses)
- LOW - immunodeficiency
- Iron
- Low iron and ferritin levels in inflammatory states, high iron feeds bacteria
- Lymphocyte Subset Panel 1 (Quest: 7197) OR T- and B-Lymphocyte and Natural Killer Cell Profile (Labcorp: 505370)
- LOW- immunodeficiency *Confirm your doctor is ordering the tests we suggest (codes to the left) as the Lymphocyte Subset Panel 3 test does not test for values that are often seen out of range in our community.
- S-100B Protein, Serum
- A calcium-binding peptide and is used as a parameter of glial activation and/or death in many disorders of the central nervous system. *This may be difficult to run. Not commonly tested.
- Serum Immunofixation (G,A,M) and Protein Electrophoresis (Includes: Proteins, IGG, IGA, IGM, and Light Chains)
- Detects and identifies monoclonal immunoglobulin gammopathies and kappa lambda light chains. They can determine if there is a paraprotein in the blood contributing to the neuropathy.
- Serum Protein Electrophoresis
- Examines specific proteins in the blood called globulins. The most common indications for a serum protein electrophoresis test are to diagnose or monitor multiple myeloma, a monoclonal gammopathy of uncertain significance (MGUS). If out of range your doctor will refer you to a hematologist, as well as aneurologist who is versed in CIDP. They can determine if there is a paraprotein in the blood contributing to the neuropathy.
- Trimethylamine N-Oxide (TMAO)
- High levels associated with vascular disease (has not been seen in our community, although we don’t believe many have tested for it.)
- Tryptase (Blood)
- Tryptase is an enzyme that is released, along with histamine and other chemicals, from mast cells when they are activated, often as part of an allergic immune response. *Tryptase is only positive in 1 out of 5 MCAS’ers. Best to test during a flare, ask for a standing order.
- Troponin (blood)
- Heart Inflammation - myocarditis. Test this if you are experiencing chest pain, heart symptoms. Usually tested in an ER.
- Thyroid Stimulating Hormone (TSH) *Best to include: Free T 3 & 4 Other hormones to consider testing are progesterone, total testosterone, free testosterone, DHEA.
- HIGH number = hypothyroid. Thyroid running too slow. LOW number = hyperthyroid. Thyroid running too fast. If out of range further labs will be ordered including anti-thyroglobulin IgG, anti-thyroid peroxidase IgG. Prolonged hyper & hypothyroidism can cause neuropathy.
- Vitamins B1, B6, B12
- Low B12, low B1 and high B6 cause neuropathy. Test fasting and before supplementing. A normal B12 test may not rule out deficiency. Some have found improvement with B12 injections or methylcobalamin liquid. -B 12 is not found in plant based foods. -B1 is only found in pork, meat, fish, seeds, nuts, tofu, squash, brown rice, asparagus, and enriched grains (thiamine will be in the ingredient list). Thiamine is usually not added to gluten free items.
- Vitamin B9 (Folate)
- Run as part of a neuropathy workup in addition to B12. Also used for red cell function and can identify anemia.
- Vitamin B12 Related Test: Methylmalonic Acid (MMA) Holotranscobalamine (Holo TC) *outside US
- MMA High level may be a sign of B12 deficiency. Holo TC is a stage 1 marker for B12 deficiency (not available in the US)
- Vitamin D
- Low levels are implicated in autoimmune, keep levels 60-100
Other:
- Glutathione
- Glutathione is essential for the immune system's proper functioning and is vital in building and repairing tissue. It acts as an important antioxidant, which helps protect your body from damage to cells caused by free radicals. *This may often be tested by an integrative doctor.
- Metals
- Mercury, arsenic, cadmium, thallium in urine have been shown in some.
*If any symptoms were predating the vaccine you may want to check this.
Imaging is usually symptom driven. No one specific imaging test is recommended.
- Cat Scan (CT)
- CNS Inflammation. Can also show clots with contrast. Many with vaccine adverse effects are sensitive to contrast medium. Weigh risk/benefit.
- Cardiac MRI
- This test will diagnose Myocarditis even if EKG and Echo are normal.
- Echocardiogram
- This test will see how well your heart is functioning. Normal LVEF 55-70
- EKG
- May assist in diagnosing myocarditis and pericarditis Learn more about diagnosing pericarditis here: https://www.mayoclinic.org/diseases-conditions/pericarditis/diagnosis-treatment/drc-20352514
- Lumbar puncture (CSF- Cerebrospinal Fluid Analysis)
- This test comes with some risk. Please weigh risk/benefit.
- MRI
- Central Nervous System (CNS) inflammation / GBS / transverse myelitis. Can show clots w/ contrast. *Many that are experiencing vaccine adverse effects are sensitive to contrast medium. Weigh risk/benefit. **MRI tests are largely coming back negative. ***Possible option is arterial spin labeling (ASL) - MRI technique. Magnetic labeling of arterial blood below the imaging slab. No gadolinium contrast needed. *No one in our community has done this test, however since gadolinium contrast has been shown to stay in the brain, and side effects have been documented, it seems a safer option.
- MRV Magnetic Resonance Venogram
- Venous thrombosis
- MRA Arteriogram
- Arterial thrombosis
- SPECT Brain Scan
- Usually not covered by insurance. Radiation exposure risk. *Similar to MRI results, not many come back with positive findings.
*Choose a neurologist or neuromuscular neurologist who performs SFN biopsy and other routine neuropathy tests including autonomic testing.
- EMG and Nerve Conduction
- Tests for large fiber involvement. Less commonly seen, but important to rule out.
**Symptoms including acute onset of progressive weakness with numbness and tingling in extremities should seek immediate evaluation for Guillain-Barré syndrome. This work up may include EMG, blood and cerebrospinal fluid analysis (CSF). Cases of slower progressive weakness should be evaluated for chronic inflammatory demyelinating polyneuropathy (CIDP). Cases among the vaccine injured have been diagnosed as GBS or CIDP that do not match the classic, textbook presentations of these diseases and have responded to traditional treatments for these diseases.
Small Fiber Neuropathy (SFN) Skin Biopsy
*Autonomic testing in Section 3 can also assist in SFN diagnosis.
Physicians How To Guide: https://react19.org/how-to-order-sfn-skin-biopsy-a-guide-for-practitioners/
“SFN occurs when damage to the peripheral nerves predominantly or entirely affects the small myelinated fibers or unmyelinated C fibers. The specific fiber types involved in this process include both small somatic and autonomic fibers.”
Link to Reference: NIH.gov Overview: In depth look at symptoms and more https://youtu.be/s66LvWQ5Qso
positive biopsy is indicative of SFN, especially when correlated with symptoms; while a negative result can be inconclusive. To increase accuracy, it has been recommended that samples be taken from highly symptomatic sites. Even when done in this manner, results may still not give the complete picture as the sample is so small. With that said, Neuropathy Commons reports a case of positive SFN ankle biopsy although symptoms were confined to the face. *If your biopsy is positive it’s important for your doctor to order tests to identify the underlying cause of your SFN(see box directly below). **If your biopsy is negative it does not rule out neuropathy. Autonomic Testing should still be ordered. (See Section 4 below.)
Columbia University lab biopsy includes tests for intraepidermal nerve fiber swelling and branching pattern changes which make the results more conclusive.
Your biopsy may be run by Therapath: Therapath Skin Biopsy Guide https://therapath.com/biopsies/skin-biopsy*Therapath does not test for qualitative alterations including intraepidermal nerve fiber swelling and branching pattern changes. “On occasion the ENFD can be normal, but the morphological examination reveals structural abnormalities such as axonal swelling or excessive branching. These are considered to be pre-degenerative changes that are also associated with small fiber neuropathy” ~Therapath Neuropathology Therapth Requisition Skin Biopsy Test Selection: https://therapath.com/wp-content/uploads/2021/09/ENFD-Requisition-12.15-Writable.pdf Confirm that your doctor has checked off each of these three tests: 1. Epidermal Nerve Fiber Density (ENFD). This test measures the density of the small sensory nerve fibers in the skin.2. Sweat Gland Nerve Fiber Density (SGNFD). This test measures the density of the small autonomic nerve fibers in the sweat glands. *This is a new test and is not typically ordered by the physician, but this option is available and relevant. https://therapath.com/sweat-gland-nerve-fiber-density/ 3. Amyloidosis and Vasculitis. These are usually run with every test, however your doctor should also check this box. If these conditions are not seen, it does not rule them out.
Your doctor will order these tests if any of your neurology tests above are abnormal; or if you have symptoms of autonomic dysfunction including gastrointestinal, bladder, bowel, heart rate, shortness of breath, or blood pressure issues.
Autonomic testing is designed to determine how well the body regulates the internal organs. During these tests, doctors use an electrocardiogram, or EKG, to monitor electrical activity in the heart and special cuffs on the fingers to continuously measure blood pressure. Orthostatic Intolerance: https://react19.org/webinar-me-cfs-dysautonomia-pots-with-dr-lucinda-bateman
Dysautonomia Basics: http://www.dysautonomiainternational.org/page.php?ID=122 Autonomic Neuropathy or Autonomic Dysfunction (Syncope) Information and Instructions: https://my.clevelandclinic.org/health/diseases/15631-autonomic-neuropathy-or-autonomic-dysfunction-syncope-information-and-instructions
POTS Testing: -Tilt Table (gold standard for diagnosing POTS) -QSART -SFN biopsy -Echocardiogram -Hemodynamic Test (Tilt w/ nuclear imaging)Hyperadrenergic POTS testing can include:- Catecholamines, fractionated, Plasma (Quest 82384) - Catecholamines, fractionated, 24 Hour Urine w/ Creatine (Quest 82384, 82570)A simple At-Home Test will give you some indication if you have POTS. -Lie down for 5 minutes. -Measure blood pressure and pulse rate. -Stand. -Repeat blood pressure and pulse rate after standing for 1 minute and 3 minutes.*If heart rate increases 30 beats over your baseline, this may be an indication of positional tachycardia. In-depth home tilt table instructions: https://batemanhornecenter.org/wp-content/uploads/filebase/providers/mecfs/10-Minute-NASA-Lean-Test-Clinician-Instructions-06_12_2022.pdf
POTS (Postural Orthostatic Tachycardia Syndrome)Learn more about POTS here: https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots
Types of POTS Syndromes: 1. Neuropathic POTS: POTS associated with damage to small fiber nerves (small fiber neuropathy). These nerves regulate constriction of the blood vessels in the legs and core body. Fatigue and low blood volume are typical. In our case this has been found in the upper body as well. 2: Hyperadrenergic POTS: Overactivity of the sympathetic nervous system. High blood pressure, “anxiety/adrenaline dumps” are common. https://youtu.be/L_b_mkapDL0 3. Low Blood Volume POTS: Reduced blood volume can lead to POTS. Low blood volume can cause similar symptoms that may overlap in neuropathic and hyperadrenergic POTS. 4. Secondary POTS: Associated with another condition known to potentially cause autonomic neuropathy, such as diabetes, Lyme disease, or auto-immune disorders such as lupus and Sjogren’s.
POTS labs/testing should include: (Per Dr. Brent Goodman, Autonomic Lab Director, Mayo Clinic) - Cbc, B12, folate, vitamin d, celiac, ANA, Ssa, complement total, C3, C4, IgA, IgM, IgG, tryptase, thyroid function, cortisol, metanephrines - Urine 11, beta prostaglandin F2, n-methylhistamine, leukotriene e4 - Consider: lupus anticoagulant, beta2 glycoprotein, antiphospholipid, paraneoplastic (autoimmune dysautonomia) panel
- Tilt Table Test - (Autonomic Test with Tilt Table)
- This test should include: 1. Heart rate deep breathing test (HRDB) 2. Valsalva Maneuver 3. Tilt Table *Tilt table testing via neurology is different from cardiology and is preferred.
- QSART (Quantitative Sudomotor Axon Reflex Test)
- Measures the autonomic nerves that control sweating. Assesses autonomic disorders, autonomic and small fiber neuropathy. *This test is only available in some states. Alternatively you can test the sweat glands via SFN biopsy and thermoregulatory sweat test.
- Thermoregulatory Sweat Test
- Tests for small fiber and autonomic neuropathies, radiculopathies, and central autonomic disorders including multiple system atrophy, Parkinson’s disease with autonomic dysfunction, and pure autonomic failure.
(If you have a positive SFN ENFD biopsy, positive SFN SGNFD biopsy, or positive autonomic testing.) *Choose a neurologist or neuromuscular neurologist who performs SFN biopsy and other routine neuropathy tests including autonomic testing.Neuropathies can be driven by an underlying condition and further testing will identify and direct potential treatments. We have listed frequently seen underlying causes, however for a complete list of possible causes please print and cross reference the tests your doctor has ordered with the following:
1. Tests for treatable causes of small-fiber polyneuropathy (Massachusetts General Hospital) - https://neuropathycommons.org/sites/default/files/Tests%20for%20SFN%20causes%2005-24-19.pdf 2. Blood Tests to Identify Medical Causes of Neuropathy - https://neuropathycommons.org/diagnosis/blood-tests 3. Testing at Washington University Neuromuscular Laboratory - https://neuromuscular.wustl.edu/over/labdis.html
*Wash U is the only US lab offering FGFR3 and TS-HDS autoantibodies. These antibodies are frequently positive in our community. Directions for link above: In the middle box, click on "serum" under "Testing at Washington U". A form will come up. We suggest, at the very least testing for everything on the "sensory panel”, as well as the other autoantibody tests in this document. *Wash U is temporarily out of materials to test TS-HDS, however you can use German lab Celltrend: https://www.celltrend.de/en/ Celltrend is not covered by US insurance. Some have completed the full Celltrend panel, however we’re not sure if these tests will be acknowledged by US doctors. Please ask the group for input. How to order Celltrend: https://react19.org/how-to-order-cell-trend-labs-for-autoantibodies/ https://www.celltrend.de/wp-content/uploads/2021/06/Patient-Instructions.pdf https://www.celltrend.de/wp-content/uploads/2021/10/Request-form.pdf
(If you have a positive SFN ENFD biopsy, positive SFN SGNFD biopsy, or positive autonomic testing.)
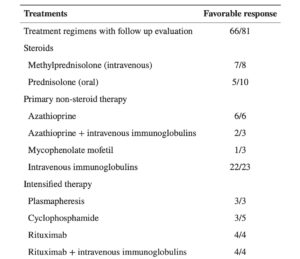
Autoimmune Dysautonomia and Immunotherapy (SFN Biopsies also discussed) - https://vimeo.com/243160944 IVIG for Auto-Immune Polyneuropathy -
https://pubmed.ncbi.nlm.nih.gov/29403541/ How We Treat Autoimmune Small Fiber Polyneuropathy with IVIG - https://www.karger.com/Article/Fulltext/498858
Current Diagnosis and Treatment of Painful Small Fiber Neuropathy - https://pubmed.ncbi.nlm.nih.gov/31773305/ Considerations for ordering autoimmune panel from CellTrend https://react19.org/how-to-order-cell-trend-labs-for-autoantibodies/
- ANCA (Antineutrophil Cytoplasmic Antibodies)
- If positive you may have autoimmune vasculitis, which can cause neuropathy. Other tests for vasculitis include biopsy of skin, nerve, muscle, cryoglobulins, HCV, RF
- Anti-Mag (Myelin associated glycoprotein)
- Learn More:https://www.hopkinsvasculitis.org/vasculitis/diagnosing-vasculitis/
“In anti-MAG peripheral neuropathy, the body produces serum IgM antibodies that bind to MAG, preventing MAG from signaling the Schwann cells and myelin to do their job. Currently, IVIG or Rituximab are the preferred treatments. Patients positive for Anti-MAG should be monitored by both a Neurologist and Hematologist as it is a neuropathy that originates in the blood.”Source: https://www.gbs-cidp.org/anti-mag/?fbclid=IwAR16yx22H0rq9vMf_IAR5I-suoYp-l3tHRbhiTJm8aIbTfW5Mh3tCkJSeeE
- Antiphospholipid Antibody Panel *Usually ordered by Rheumatologist
- Many with Sjogren’s have an antiphospholipid antibody positive (Per Dr. Brent Goodman, Neurologist, Mayo Clinic).
- - Anti-c1q igG - Anti-Ribosomal P IgG - Anti-Phosphatidylserine/Prothrombin IgM and IgG - Anti-Cardiolipin IgM, IgG, IgA - Anti-B2 Glycoprotein 1 IgM, IgG, IgA
- 50% of people with Lupus possess these antibodies.People w/o Lupus can also have these antibodies. People that have complications from these antibodies are diagnosed with APS (Antiphospholipid Syndrome) which cause blood platelets to clump together.
- Anti-NDMA-R Antibodies
- “These antibodies disrupt brain signaling and cause brain swelling, or encephalitis.” Can cause neuropathy. *At present, only 1 person has tested positive in our community.
- FGFR3 (Fibroblast Growth Factor Receptor)
- Washington University is the only lab offering this test.https://neuromuscular.wustl.edu/over/labdis.html In the middle box, click on "serum" under Testing at Washington University. A form will come up. We suggest testing for everything on the "sensory panel”. A positive result has assisted some people with IVIG approval. *Doctor and insurance dependent.
- Gad-65 (Glutamic Acid Decarboxylase)
- Gad-65 antibodies can cause Small Fiber Neuropathy. This test can be performed by most labs including Washington University (see form above, “Other Tests” section.) Gad-65 is often associated with Stiff Man Syndrome (which has not been found among the neurological adverse effects group), however your doctor may be able to use this positive lab to get IVIG approved.
- Ganglioside Antibody Panel Quest, Test Code 90131 (Ganglioside Antibody Panel) 1. Ganglioside GM-1 Antibodies (IgG, IgM), EIA 2. Ganglioside GD1a Antibody (IgG, IgM), EIA 3. Ganglioside Asialo-GM-1 Antibody (IgG, IgM), EIA
- Immune mediated peripheral neuropathy, GBS *This positive lab result may also qualify you for IVIG if this treatment is considered appropriate by your treating physician.
- Lupus *Usually ordered by Rheumatologist
- Lupus can cause peripheral neuropathy. Lupus anticoagulant panel. Your tests may include: ANA, dsDNA antibodies, SCL-70 antibodies, Sm antibodies, RNP antibodies, biopsyhttps://avisetest.com/provider/ctd/ for reference.
- LYME (B. Burgdorferi)
- Lyme can cause peripheral neuropathy. Labs can show positive and then negative at times. Western Blot has been the most used testing method. Igenex.com has been suggested by some.
- PANS/PANDAS
- Pediatric Autoimmune Neuropsychiatric Disorders. https://pandasnetwork.org/understanding-pandas/ ** A few adults in our groups have been given this diagnosis
- Sjogren’s SS-A (Ro), SS-B (La) *Your Neurologist should include Sjogren’s testing, however these tests can also be ordered by your Rheumatologist.
- -Sjogren’s is a cause of Small Fiber Neuropathy and Axonal Neuropathy. -Negative Sjogren’s test does not rule out Sjogren’s. *https://www.youtube.com/watch?v=N77sfyQB63A-90% of Sjogren’s SS-A and SS-B negative results are false. (Per Dr. Brent Goodman of the Mayo Clinic) -Some patients with Sjögren’s syndrome have elevated levels of immunoglobulins IgA, IgG, IgM, and can be hyperglobulinemia, reflecting overactivity of the immune system. (Per John Hopkins) -IgG Subclasses may be low.
Sjogren’s can be treated with Intravenous Immunoglobulins (IVIG) and/or steroids. (Per neurologist Dr. Levine) -If you have a positive test, your insurance company may want you to try immunosuppressive drugs, or hydroxychloroquine before IVIG. Sjogren’s possible treatments- Learn more https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6637792/
- Sjogren’s Lip Biopsy
- Picks up 73% of cases. Negative results do not rule out Sjogren’s. -There is a chance the lip biopsy can cause permanent numbness. -If you have a positive test, your insurance company may want you to try immunosuppressive drugs, hydroxychloroquine before IVIG. -Please research and weigh the risk/benefit of the test and possible treatments.
- Sjogren’s Early Profile
- A positive will not prompt a Sjogren’s diagnosis, but can be useful as according to some, 90% of Ro and La negatives are false.
- TNF Alpha
- Protein that causes inflammation, implicated in autoimmune disease.
- TS-HDS (Trisulfated heparin disaccharide)
- Associated with Small Fiber Neuropathy. Celltrend is currently the only lab testing this antibody. The only US lab (Wash U) cannot performs this test at the presnt time due to backorder of reagents from supplier. A positive result may assist you in obtaining insurance approval for IVIG, however this is insurance and doctor dependent.
Reactivation of latent viruses have been seen in our community, and many can cause neuropathy.Complications from these viruses are more likely seen in the immunocompromised. **If positive, please check that you're not immunodeficient by running IgG subclasses and T and B Lymphocytes with Natural Killer Cells.
- Cytomegalovirus (CMV/member of herpes virus family)
- Rule out active infection, reactivation of latent virus.
- COVID (Nose/ Saliva)
- Acute COVID - There have been reports of worsening of neurological symptoms especially neuropathy during and after COVID infection. In many cases, the symptoms return to baseline.
- Epstein Barr Virus Antibody Tests (EBV/ Herpes Virus 4)
- Rule out acute virus and reactivation of latent virus. Can cause mononucleosis. More here: https://www.medscape.com/viewarticle/553327_5 -Viral Capsid Antigen (Anti-VCA IgG) antibodies indicates that an EBV infection has occurred at some time recently or in the past. -Viral Capsid Antigen (Anti-VCA IgM) antibodies, and the absence of antibodies to EBNA mean that the infection has occurred recently.-Early Antigen EA (Anti-EA IGG) appears in the acute phase of the infection, although in 20% of healthy people they can be present for life. -EBV Nuclear Antigen (EBNA) means that the infection occurred in the past. Antibodies to EBNA develop six to eight weeks after the time of infection and are present for life.
- Herpes Simplex
- Rule out active infection, reactivation of latent virus
- HHV-6A and HHV-6B
- Rule out active infection, reactivation of latent virus More here: https://hhv-6foundation.org/what-is-hhv-6
- Lyme
- Rule out infection/Reactivation
- Mycoplasma
- “The subspecies mycoplasma pneumoniae is the most widely studied and although it is typically associated with "atypical pneumonia" it can also lead to infections of other anatomical sites such as skin, central nervous system, blood, heart, and joints.” https://www.ncbi.nlm.nih.gov/books/NBK536927/
- Nucleocapsid Blood Test
- Past Covid–As a “Long Hauler” the door may be opened to more clinicians.
- Varicella Zoster (Chicken Pox Virus/member of the herpes family)
- Can cause Shingles (which can cause neuropathy and neuralgia).
- Colonoscopy and Endoscopy
- Consider this test if experiencing symptoms.
- SIBO (Small Intestinal Bacterial Overgrowth)
- SIBO and other gut conditions can cause dysbiosis (gut imbalance) which can lead to histamine intolerance. *Symptoms: bloating, gas, cramps
Trio-Smart
https://www.triosmartbreath.com/prescribers
https://www.triosmartbreath.com
Trio-Smart is the only clinical breath test that measures hydrogen sulfide. -You may want to have your physician order the Lactulose Substrate (easy to ingest) instead of the glucose liquid (requires ingesting a large bottle of artificially flavored liquid) that comes with the test. -You may want to have your physician order the Lactulose Substrate (easy to ingest) instead of the glucose liquid (requires ingesting a large bottle of artificially flavored liquid) that comes with the test. -While you can order this test on the site without a doctor (the order generated by this site is signed by a physician), we suggest checking with your insurance company to confirm coverage. -If positive you will require a gastroenterologist to prescribe medication. (Confirm that prescribed antibiotics/drugs do not cause neuropathy.) -Current research suggests that NAC taken with antibiotics make the medication more effective as it assists in getting the medication into the gut lining. -If the test is positive, we make a strong recommendation for the book, “The Microbiome Connection” by Dr. Mark Pimentel. It contains information on motility which may be helpful to those with autonomic dysfunction.
Acid Reflux or GERD How to do a simple at home test to determine if you have too much acid or not enough acid: -First thing in the morning (before eating or drinking), mix 1/4 teaspoon of baking soda in 4 ounces of cold water. -Drink the baking soda solution. -Set a timer and see how long it takes you to burp. If you have not burped within five minutes, stop timing. If your stomach is producing adequate amounts of acid you’ll likely burp within 2 -3 minutes. Any burping after 3 minutes may indicate low acid level.If you don’t have enough acid we have heard that adding Better Bitters Spray by Herb Pharm, and possibly Betaine HCL as needed will be helpful. If symptoms worsen please discontinue.
Doctors often suggest proton pump inhibitors (PPIs) to control acid when the real issue is an inadequate amount of acid.*Long-term Use of PPIs can disrupt the microbiome, consult with your physician.*Many in our community are consuming Pepcid (famotidine). It works by decreasing the amount of acid your stomach makes. If you don't have enough acid, the food in your gut will ferment further causing gut and histamine issues.
If your stomach is producing adequate amounts of acid you’ll likely burp within 2 -3 minutes. Burping after 3 minutes, or no burping may indicate low acid level.
If you don’t have enough acid we have heard that adding Better Bitters Spray by Herb Pharm, and possibly Betaine HCL as needed will be helpful. If symptoms worsen please discontinue.
It’s possible to have a histamine intolerance without having Mast Cell Activation. Some patients experience a benefit from MCAS therapeutics without any positive MCAS testing. While some in our community have tested positive for MCAS (with a Tryptase test), it is theorized that most have a temporary histamine intolerance caused by either an immune system response, or gut dysbiosis. *Some tests below are temperature sensitive. Follow lab directions carefully.
Beginner’s General Review of MCAS: https://www.legalnomads.com/mast-cells MCAS Diet: https://www.mastzellaktivierung.info food list pdf Histamine Intolerance Fact Sheet - Dr Tina Peers: Histamine Intolerance Fact Sheet (pdf) MCAS and Brain Disorders: https://www.courtneysnydermd.com/blog/mast-cell-activation-inflammation-in-brain-disorders-how-to-calm-things-down?
- Tryptase (Blood)
- Negative result does not rule out MCAS. Many people only had positive results when tested in the middle of a flare.
- HATS gene
- Individuals with a consistently elevated Tryptase level should test for the genetic variant, HATs.
- Hereditary Alpha Tryptasemia Syndrome
- Genebygene.com is the only company that performs the TPSAB1 gene test. $200. Unless you have chronically elevated Tryptase you are unlikely to have HATS variant, however it has been found that 8% of patients without an elevated Tryptase level have been found to have redundant TPSAB1 HATS gene. We are not making a recommendation for the company Gene By Gene for whole genome sequencing. If your tryptase level is elevated because of the HATS gene, online resources say that you would not need to be in a flare to have a positive Trypatse test. Confirm with your doctor.
- Histamine, 24-Hour Urine (Quest 4946)
- TOTAL VOLUME: 800
- 2,3-Dinor-11 Beta-Prostaglandin F2 Alpha, 24 Hour, Urine (Quest 10109)
- CREATININE, 24 HOUR, U - COLLECTION DURATION: 24HR, Urine Volume 800ML
- Prostaglandin PGD2 (Quest 10180)
- Inflammation. Often run as part of a 24 hour urine.
- Leukotriene E4, 24 Hour, Urine (Quest 11976)
- CREATININE, 24 HOUR, U - COLLECTION DURATION: 24HR, Volume 800ml
- Colonoscopy
- If you’re having a colonoscopy for gut issues, it’s a great time to rule out MCAS. Biopsy during colonoscopy is one of the most reliable methods of testing for MCAS, although bone marrow biopsy may be more accurate. If you are having a colonoscopy and you’d like to check for MCAS, here is a sample of an immunologist’s request to a gastroenterologist: “Evaluate for mast cells with stains for CD117, CD25, CD2 as well as CKIT mutation (Codon 816 mutation). Also assess for aggregates of mast cells within the biopsy as well as if greater than 25% of mast cells are immature, atypical mast cells, or spindle shaped mast cells.”
Persistent allergic response has been found to be more common in our communities. Ruling out clinical MCAS, food and other allergies is important.
- Immunoglobulin E (IgG)
- Helps rule out persistent allergic responses.
- Immunoglobulin G (IgG)
- IgG Food Antibody Assessment - measures antibodies to 87 commonly consumed foods. Full panel also includes an IgE measurement.
- CU Index
- Chronic urticaria (hives, rash, itchy rash, welts) is a common disease in which most cases were considered to be idiopathic. Recent evidence indicates that at least a subset of cases of chronic idiopathic urticaria are autoimmune in origin.
- Eosinophils
- Elevated in response to an allergy
- RAST testing
- This test shows the amount of IgE antibodies to an allergen.
- Serum histamine and 24 hour urine histamine
- This test can indicate a histamine intolerance
- Skin Prick
- Food Allergy and environmental allergies. Must be off all antihistamines for proper testing. Some say Benzos are also a mast cell stabilizer. Please do your own research.
- MTHFR - Genetic Marker
- Having one or two MTHFR mutations can slightly increase the levels of homocysteine present in the blood. This condition is called homocysteinemia. Homocysteine is an amino acid that the body produces by breaking down dietary proteins. Having high levels of homocysteine can damage blood vessels and lead to blood clots.
- Porphyria - Genetic Marker
- Buildup of certain chemicals that affect red blood cells
- IVCM
- Noninvasive corneal microscopy test for small fiber neuropathy
(See Action Plan on page 1 for full list of conditions to rule out)
- ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome )
- ME/CFS Crash Guide - Survival Handbook -https://batemanhornecenter.org/education/mecfs-guidebook/ Diagnostic Criteria found here: https://batemanhornecenter.org/wp-content/uploads/filebase/Diagnosing-and-Treating-MECFS-Handout-V2.pdf
- EDS - Ehlers-Danlos Syndrome
- People with Hypermobility / EDS are at higher risk of suffering a reaction. At-Home tests can identify possible EDS (hypermobile). The Beighton Scale can be an easy test to identify this syndrome
*Highly unlikely these tests will be covered by insurance. These additional tests are optional and not pivotal in guiding your care. An integrative doctor may be required to order these tests and interpret them for you. We are not making a recommendation for these tests, however some have found them useful.
- Cellular Micronutrient Assay
- https://www.vibrant-america.com/micronutrient/ Infections. 12 Pathogen Associated Immune Reactivity Screen ($379) https://www.cyrexlabs.com/CyrexTestsArrays This test cannot distinguish between past or current exposure. If markers for viral activation are elevated, additional testing is advised. Or skip this test and have your doctor run tests for these viruses/bacteria. Please research.
- GI Map Test
- Diagnostic Solutions-Diagnostic GI Map. This test identifies imbalances in the gut microbiome. https://www.diagnosticsolutionslab.com/tests/gi-map *Recent studies show that the gut microbiome is changed with the food you eat. According to IBS research leader, Dr. Mark Pimentel and many gut integrative specialists, Bifido seems to be the only probiotic that has been shown to help. Many probiotics may exacerbate histamine issues. Please do your own research.
- Vibrant America Mycotoxins Test $360
- Environmental toxins (chemicals, mycotoxins, heavy metals) https://www.vibrant-wellness.com/tests/mycotoxins/ 8May not differentiate between present and past exposure.
- Chemical Immune Reactivity Screen $295
- Cyrex Labs, Array 11 https://www.cyrexlabs.com/CyrexTestsArray
- Cytokine/Chemokine Profile
- IncellDx or Standard Lab. Elevated cytokines/chemokines are not a diagnostic tool, however almost all in our community have elevated cytokines/chemokines. Cytokines and chemokines fluctuate in a typical patient at any given time.
- sCD40L and VEGF
(Soluble CD40 Ligand and Vascular Endothelial Growth Factor) - IncellDx Cytokine panel and other labs.Not a diagnostic tool. May indicate vascular inflammation, Lupus, rheumatoid arthritis, Sjogren’s, cancer and other diseases. *Statins can increase VEGF levels.
This document is for informational purposes only. This list was not written by a medical institution or doctor. This list is not intended to diagnose, treat, cure or prevent any disease. The considerations offered in this guide do not replace the medical interventions prescribed by the user’s care team and should be evaluated prior to implementation. Consult with your trusted provider.
Contributors: Brian Dressen PhD, Shaun Barcavage NP, Nancy Valen, Julia Marks RN BSN, Danice Hertz MD, Jeanne Marie
